Use Your Diet to Help Tame Irritable Bowel Syndrome
Answer a few questions and we'll provide you with a list of primary care providers that best fit your needs.
What you eat can help control the symptoms of irritable bowel syndrome.
This chronic condition affects up to 20 percent of Americans and can cause problems such as:
- Abdominal pain
- Gas and bloating
- Changes in bowel habits, such as diarrhea or constipation
Doctors think irritable bowel syndrome is caused by overactive or abnormal contractions of the colon. The condition can occur at any age, and symptoms may be triggered by an infection.
Irritable bowel syndrome is the second-leading cause of absence from work in the United States. It’s an issue that people are more comfortable talking about in recent years.
What You Eat Matters
While many factors affect irritable bowel syndrome, diet can be critical.
Your body may have trouble digesting certain foods. If stress or changes in hormones trigger your IBS, certain foods can intensify symptoms.
IBS is related to overactive muscles and nerves in the colon, and the simple act of chewing can aggravate symptoms by releasing hormones that stimulate the gut.
Making diet and lifestyle changes are two of the best ways to control your irritable bowel symptoms.
Be sure to talk with your doctor before making serious changes. The signs of irritable bowel syndrome can mirror many other conditions, such as Crohn’s disease or ulcerative colitis. Your doctor will want to rule out other ailments and may use tests such as a lower gastrointestinal scope to make a diagnosis.
Irritable bowel syndrome is the second-leading cause of absence from work in the United States.
Making Dietary Changes
Different foods affect those with IBS differently. As you work to determine what triggers your symptoms, keep a diary of what you eat. Make note of which foods and drinks bother you.
In general, eating more fiber and avoiding gluten often helps relieve the pain, gas and bloating of IBS. It may take several weeks before you notice an improvement in your IBS symptoms.
Fiber. Fiber makes stools softer. Adults should eat 22 to 34 grams of fiber a day. Soluble fiber, contained in beans, fruit and oat products, helps relieve IBS symptoms. Add more fiber to your diet slowly, upping the amount by 2 to 3 grams a day. Too much fiber at once can cause gas and trigger IBS symptoms.
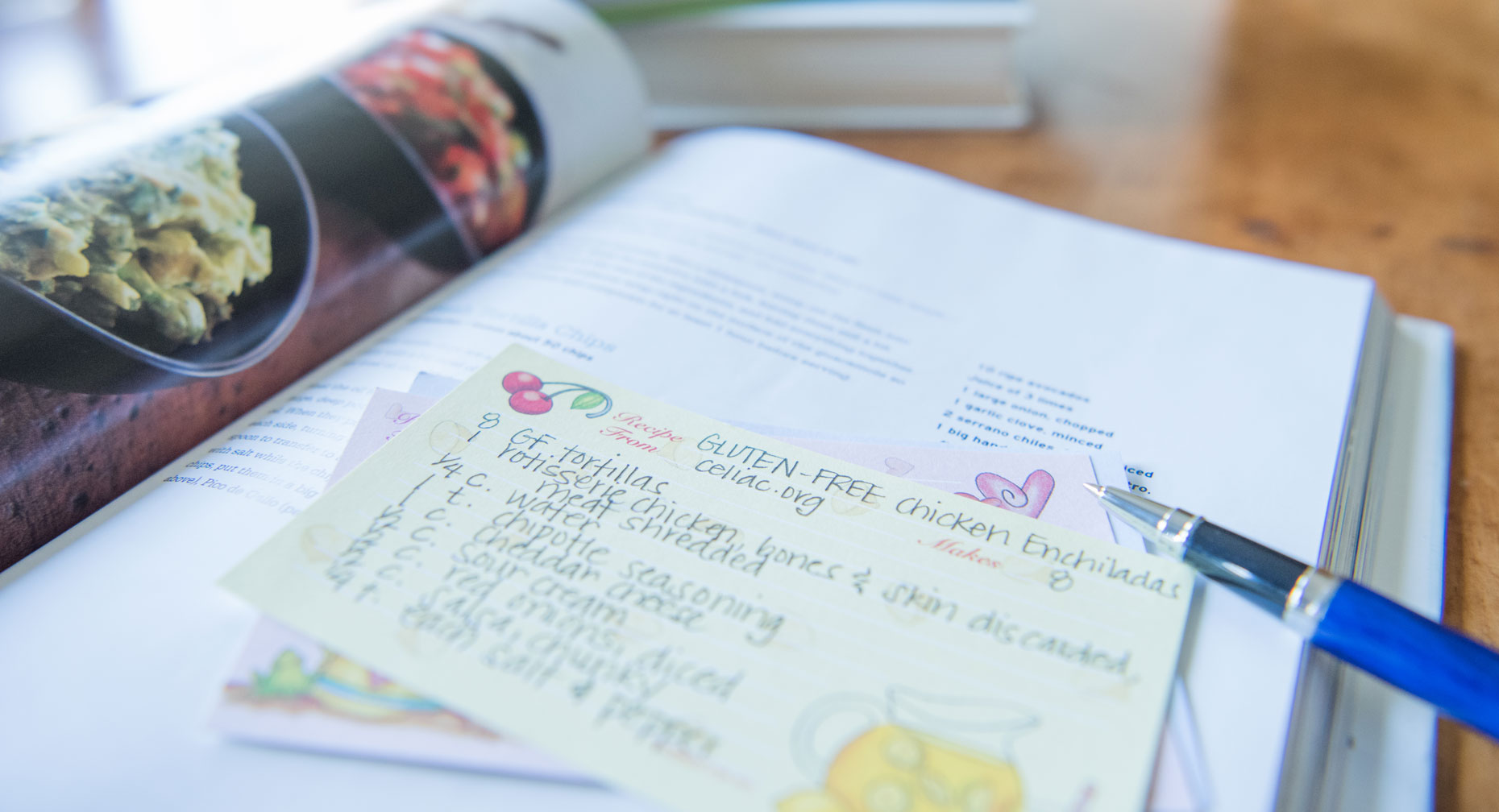
Avoid gluten. Some people with IBS experience symptoms after eating foods with gluten, even though they do not have celiac disease (gluten intolerance). Gluten is a protein found in barley, rye and wheat. Processed foods, cereals, grains and pasta contain gluten.
The Low FODMAP Diet

Depending on your symptoms and how your body responds to more general diet and lifestyle changes, your doctor may recommend that you follow a low FODMAP diet.
FODMAP stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides and Polyols. Simply put, these are types of carbohydrates that are hard to digest.
Foods to avoid on the low FODMAP diet include:
- Fruits such as apples, apricots, blackberries, cherries, mango, nectarines, pears, plums and watermelon. Also, juice containing any of these fruits.
- Canned fruit in natural fruit juice, or large amounts of fruit juice or dried fruit
- Vegetables such as artichokes, asparagus, beans, cabbage, cauliflower, garlic and garlic salts, lentils, mushrooms, onions, and sugar snap or snow peas
- Dairy products such as milk, milk products, soft cheeses, yogurt, custard and ice cream
- Wheat and rye products
- Honey and foods with high-fructose corn syrup
- Candy, gum and other products with sweeteners ending in “–ol,” such as sorbitol, mannitol, xylitol and maltitol
Foods in the FODMAP group are not absorbed well by the small intestine. This creates gas and more fluid in the bowel, which leads to IBS symptoms. In one research study, 76 percent of patients who followed a low FODMAP diet experienced an improvement in their symptoms, Harvard Health reports.
Foods to eat more of on the low FODMAP diet include:
- Fruits such as bananas, blueberries, cantaloupe, grapefruit, honeydew, kiwi, lemon, lime, oranges and strawberries
- Vegetables such as bamboo shoots, bean sprouts, bok choy, carrots, chives, cucumbers, eggplant, ginger, lettuce, olives, parsnips, potatoes, spring onions and turnips
- Dairy products such as lactose-free milk, rice milk, almond milk, coconut milk, lactose-free yogurt, and cheeses such as feta and brie
- Protein such as beef, chicken, eggs, fish, pork and tofu
- Nuts/seeds (limit to 10-15 each) such as almonds, macadamia, peanuts, pine nuts and walnuts
- Grains including oat, oat bran, rice bran, gluten-free pasta (such as rice, corn, quinoa), white rice, corn flour and quinoa
If your symptoms improve on the low FODMAP diet, your doctor may recommend that you slowly reintroduce some foods that contain FODMAPS. You may tolerate some foods better than others and you may be able to eat certain foods on the “avoid” list without getting IBS symptoms.
Answer a few questions and we'll provide you with a list of primary care providers that best fit your needs.
Source: National Institutes of Health; Harvard Health; International Foundation of Functional Gastrointestinal Disorders; Diet and Lifestyle Tips for Irritable Bowel Syndrome (IBS), Staywell Kra




